
In our hustle-driven culture, burnout is often seen as a badge of honor—proof of dedication, ambition, and productivity. But beneath this glorified narrative lies a dangerous truth: unmanaged stress doesn’t just sap your energy; it systematically undermines your long-term health. Burnout is more than mental exhaustion; it’s a warning sign that your body is under siege.
Understanding Burnout
Burnout is a state of chronic physical and emotional exhaustion brought on by prolonged stress, typically related to work or caregiving. It manifests through feelings of cynicism, detachment, and a sense of ineffectiveness. When left unaddressed, burnout becomes more than a psychological state—it begins to erode your physical well-being.
The Health Consequences of Long-Term Stress
Stress in small doses is a natural and necessary part of life. But when stress becomes a constant companion, it triggers a cascade of health issues that can become chronic and life-altering.
1. Cardiovascular Risks
One of the most well-documented outcomes of chronic stress and burnout is heart disease. Stress elevates blood pressure and heart rate, damages artery walls, and promotes inflammation. Over time, this increases the risk of hypertension, arrhythmias, heart attacks, and stroke.
2. Immune System Suppression
Constant stress impairs the immune system’s ability to function effectively. This makes the body more susceptible to infections and slows down the healing process. Long-term immune suppression can also increase vulnerability to autoimmune diseases and certain cancers.
3. Neurological and Cognitive Decline
Prolonged exposure to stress hormones like cortisol can damage areas of the brain responsible for memory and learning, such as the hippocampus. This can lead to forgetfulness, difficulty concentrating, and increased risk of neurodegenerative diseases like Alzheimer’s.
4. Endocrine and Metabolic Disruption
Burnout often disrupts hormonal balance, particularly in the adrenal glands. Chronic cortisol elevation can lead to insulin resistance, abdominal obesity, and metabolic syndrome—all risk factors for type 2 diabetes and other metabolic disorders.
5. Gastrointestinal Problems
Stress alters gut motility and increases stomach acid production, contributing to conditions like acid reflux, ulcers, and irritable bowel syndrome (IBS). The gut-brain connection also means stress can worsen or even trigger digestive issues.
6. Sleep Disorders
Chronic stress interferes with sleep patterns, causing insomnia or restless sleep. Poor sleep further amplifies stress levels, creating a vicious cycle that leaves the body and brain unable to recover properly.
Strategies for Recovery and Prevention
Managing stress isn’t just a matter of mental wellness; it’s critical for physical health. Here are practical steps to address burnout:
- Set clear boundaries: Protect your personal time and space.
- Adopt stress-relief practices: Meditation, deep breathing, and yoga are proven to reduce stress levels.
- Maintain social connections: Supportive relationships buffer the effects of stress.
- Prioritize self-care: Regular exercise, nutritious meals, and sufficient sleep are essential.
- Seek professional help: Counseling or therapy can provide tools and insights for recovery.
Final Thoughts
Burnout is not just a phase—it’s a warning. Ignoring chronic stress can lead to irreversible health consequences. Recognizing the long-term risks and taking proactive steps toward recovery isn’t just good practice; it could be life-saving.





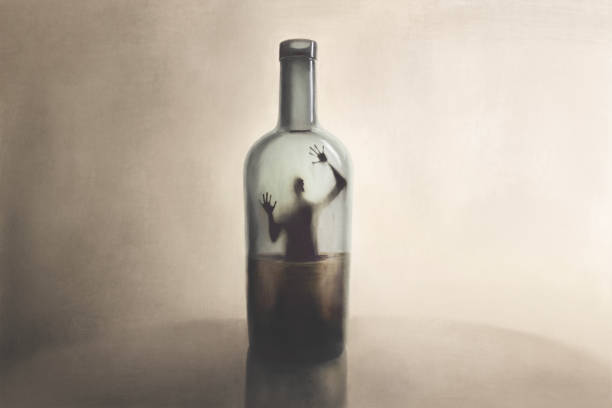
 One of the first steps in the mental health recovery process is to recognize the problem. People often find it difficult to come to terms with the fact that they have a mental health issue, so recognizing the symptoms and confronting them is important. It is also essential to speak to a medical professional and get an accurate diagnosis so that the right treatment plan can be created.
One of the first steps in the mental health recovery process is to recognize the problem. People often find it difficult to come to terms with the fact that they have a mental health issue, so recognizing the symptoms and confronting them is important. It is also essential to speak to a medical professional and get an accurate diagnosis so that the right treatment plan can be created.